A commentary for International IDEA’s website
As COVID-19 virus infections are spreading across the world, the factors enabling states to cope with the pandemic have become the subject of intense public debate. High-income countries can rely on a much more developed hospital infrastructure to treat patients in critical conditions. However, economic wealth is not the only factor influencing the response capacities of states. China has demonstrated that it is possible to limit the spread of the disease by enforcing strict measures of social distancing and isolation.
China’s apparent effectiveness and the dramatic increases in mortality rates in some democratic countries have raised doubts as to whether democracies are well equipped to address the challenges posed by COVID-19. Democracies may not use social surveillance methods to track infections among their citizens, and they are less able to constrain the civil liberties on which they are built. To impose far-reaching emergency measures in democracies, governments need to comply with constitutional rules and persuade political and institutional veto players. These perceived weaknesses have been exploited by some governments to monopolize executive powers in the name of effective crisis management, for example in Hungary.
However, there is no empirical evidence proving an inherent weakness of democracies in managing the impact of the pandemic. International IDEA staff has analyzed how the democratic quality of states is related to the effectiveness of their health systems in containing the number of case fatalities. This analysis draws on the Global State of Democracy Indices (GSoDI), a large data set measuring aspects of democracy in 158 states. The most recent GSoDI update reflects the situation in 2018. To assess the effectiveness of the policy response to the pandemic, the analysis focused on the share of COVID-19-related deaths as a percentage of confirmed infections. Lower mortality rates can be viewed as approximate indications of more effective policies.
The underlying numbers of confirmed infections and deaths are taken from a database established by the Coronavirus Resource Center at Johns Hopkins University. This database provides daily updates on the scope of infections in a large number of countries, based on sources from the World Health Organization, various national health authorities and other organizations. The cross-national comparability of the figures is limited since individual national health authorities vary in their approaches to identifying and registering COVID-19 cases. Yet their broad coverage is of great value for grasping the pandemic in its national trajectories.
The analysis has examined how different aspects of democratic quality correlate with fatality rates reported in countries during the third week after a local outbreak, which was defined as the first day with the number of confirmed infections exceeding 100. Rather than choosing a fixed date, these country-specific timelines reflect the fact that countries are at different stages of the epidemic curve. On 31 March 2020, 47 countries had passed 14 days after the local outbreak. Of these countries, 36 are classified as democracies and 11 are viewed as non-democracies or hybrid political regimes by the GSoDI. To account for day-to-day fluctuations in mortality rates, three-day moving averages were calculated.
Among the 28 aspects of democracy measured by GSoDI, an impartial public administration, basic welfare, and personal integrity/security are most strongly correlated with lower fatality rates. These patterns tend to confirm the importance of economic wealth and state capacity, but also show that political regimes protecting personal security tend to perform better. Within the subset of democracies, civic engagement was most consistently correlated with lower rates. Labeled Civil Society Participation in the GSoDI, this aspect measures the extent to which societies are characterized by organized, voluntary, self-generating and autonomous civic associations. The plot below shows the COVID-19 fatality rates of democracies at different levels of Civil Society Participation (ranging from 0 to 1 = highest).
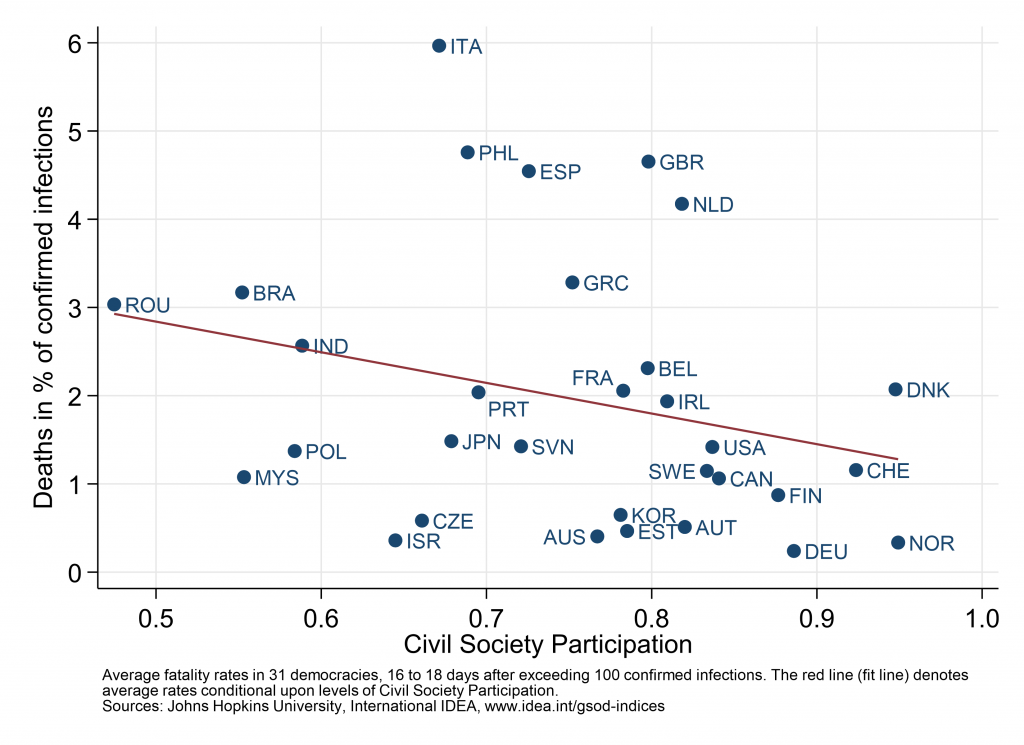
The graph represents only a snapshot of an early moment in the global struggle against the pandemic. However, the negative correlation indicates that both the engagement of citizens in civil society organizations and the involvement of civil society in public policy-making are associated with better performance on a crucial indicator of public health. There may be different causal mechanisms at work here: citizens experiencing that their voice matters in the public sphere are likely to trust more in government and behave responsibly; civil society organizations acting as transmitters, supporters and amplifiers of public health policy measures; or civic engagement and dense associational networks contributing to interpersonal trust and more solidarity with vulnerable groups. These and other possible causal pathways linking civic engagement to a flatter epidemic curve and lower fatality rates need to be further explored. Further research is also necessary to assess whether antecedent or confounding causal factors shape the relationship or whether it will persist as the pandemic unfolds further.
However, there is enough reason for skepticism as to whether a narrow understanding of state capacity as the ability to enforce drastic emergency measures will be key to master the current crisis. The pattern from the early days of the COVID-19 crisis points to a source of resilience in democracies and a competitive advantage. Their governments may lag behind authoritarian regimes in implementing unpopular measures, but they are better positioned to engage civil society for public policies.